Dr. Kevin Dzobo, NEF Fellow
Scientists and clinicians, motivated by the need to develop safe and reliable sources of tissues and organs, have been developing therapies and technologies that can be used to create or regenerate tissues and organs. Regenerative medicine and /or tissue engineering are fields of life science employing both engineering and biological principles to promote the regeneration of damaged or diseased tissues, using stem cells and 3D bioprinting.
The regenerative power of stem cells mean that, given the right cue, they can be differentiated into many types of tissues and organs. Already there has been promising results for the regeneration of the skin, heart, kidney, liver and congenital flaws. As well, stem cells are being used to treat several conditions such as multiple sclerosis, leukaemia, cancer and diabetes. And this is just the beginning.
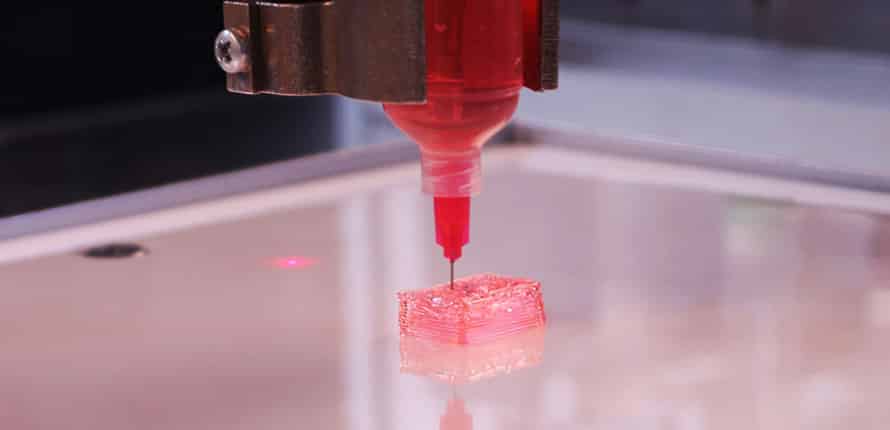
One of the most impressive and disruptive technological advancement of the last decades is 3D printing and more specifically, 3D bioprinting. Successful bioprinting requires the proper placement of biological material, cells and biomolecules such as growth factors. In order to mimic human tissue, 3D bioprinting must be able to capture the complex structure and organization of the extracellular matrix (ECM) and all the multiple cells present in tissues and organs. 3D bioprinted tissues and organs must be able to recapitulate the vascular system and the nervous system of each tissue and organ needed.
From its humble beginnings, being used in the manufacturing and engineering industry, 3D printing is now driving innovations in medicine. It is estimated that by 2027, the 3D bioprinting global industry will be worth close to 55.8 billion dollars (1). Complex functional tissues comprised of biomaterials, stem cells and biomolecules have been printed. In addition, the ability to reprogram and use patient-specific cells during 3D bioprinting allows for personalized tissue and organ printing.
There are a multitude of success stories of people’s lives being saved by stem cells and 3D bioprinting. Already healthcare transformation is taking place through the 3D printing of prosthetics and hearing aids for example. The cost of 3D printing these medical devices is at a fraction of the traditional devices. A story of a baby born with a severely weak airway tissue, saved by a 3D printed a scaffold-like tube to hold his airways open is another example.
The US Food and Drug Administration has approved the 3D printing of drugs such as Spritam, a drug 3D printed with layers of powder and liquid droplets. This allows the drug to dissolve fast. In the future, it is possible that instead of taking many pills a day patients will take just one 3D printed pill, a combination of all the required pills. Imagine visiting a pharmacy with a prescription and the pharmacist will 3D print composite pills, consisting of all your daily drugs. Developing countries will benefit immensely because as along as the ingredients are there, 3D printing can happen anywhere in the world, cutting costs as shipping and tariffs are removed.
Further, 3D bioprinted tissues and organs can be used for testing new drugs and therapies. Because bioprinted tissues and organs are made from human stem cells and natural materials, they can better predict clinical outcomes. This could potentially remove the need for animal testing.
The next 10 years are going to be defining for stem cells and 3D bioprinting. Technological advances will allow for the fabrication of patients specific and tailor-made grafts that will position stem cells within specific regions of the scaffold and possibly mimic native tissues. Most importantly graft integration with host tissue will improve with new knowledge on graft vascularization and nerve formation. Increased knowledge on stem cell behavior mean controlled differentiation of the stem cells can be achieved, allaying fears of their safety.
Through our research we hope to produce a stem cell-ECM patch which is a mixture of stem cells and natural extracellular matrix. We hope this will aid and speed up the healing of damaged tissue and in our case damaged cartilage. Damages to the knee cartilage is a major challenge for many people. Currently, cartilage damage is fixed through drilling into the bone to release stem cells that can help heal the nicks. The process is a horribly invasive one. We hope that our stem cell-ECM patch can help fill cartilage gaps or wounded areas with the scaffold or natural extracellular matrix full of adipose derived stem cells (2). These cells are obtained from fat tissues, usually discarded as medical waste. The patch can be molded into different shapes depending on the damage on the cartilage.
With our collaborators we hope to come up with natural-inspired extracellular matrices that can improve the synthesis of new cartilage by the stem cells and also exploring ways to 3D bioprint the patch. Our hope is that the scaffold or extracellular matrix will dissolve away leaving perfect tissue in place. The cells used in the patch can come from the person, making personalized regenerative medicine possible.
Healthcare has already been dramatically changed by stem cells and 3D bioprinting. For the field of regenerative medicine to achieve its goals, it is going to require the coming together of scientists from the medical continuum and others such as engineering and physics. Long-term and stable funding is going to be necessary before we can enjoy all the benefits of regenerative medicine. With stem cells and 3D bioprinting, the possibilities are endless!
Stem Cells and 3D Bioprinting: Game changers in Medicine of the 21st century
February 19, 2018